Abstract
Background:
The management of older patients with Myelodysplastic syndrome (MDS) and Acute Myeloid Leukaemia (AML) is currently based on disease biology and performance status despite the heterogeneity of ageing and the increasingly complex care needs of frail and multi-morbid patients. Performance status scores fail to capture deficits across all the domains of ageing therefore patients that are pre-frail or vulnerable fail to be identified early in their journey. Geriatric assessments have been firmly established in the management of oncological patients but not as yet in haematological malignancies.
Aims and Methods:
This prospective interventional study was conducted at the Royal Adelaide Hospital. The aim was to determine if deficits in ageing were associated with therapy completion rates and survival. After the treatment decision had been made by the haematologists, consented patients had nurse-led geriatric assessments followed by Geriatrician review in participants with abnormal assessments subjective concerns with interventions implemented.
Results:
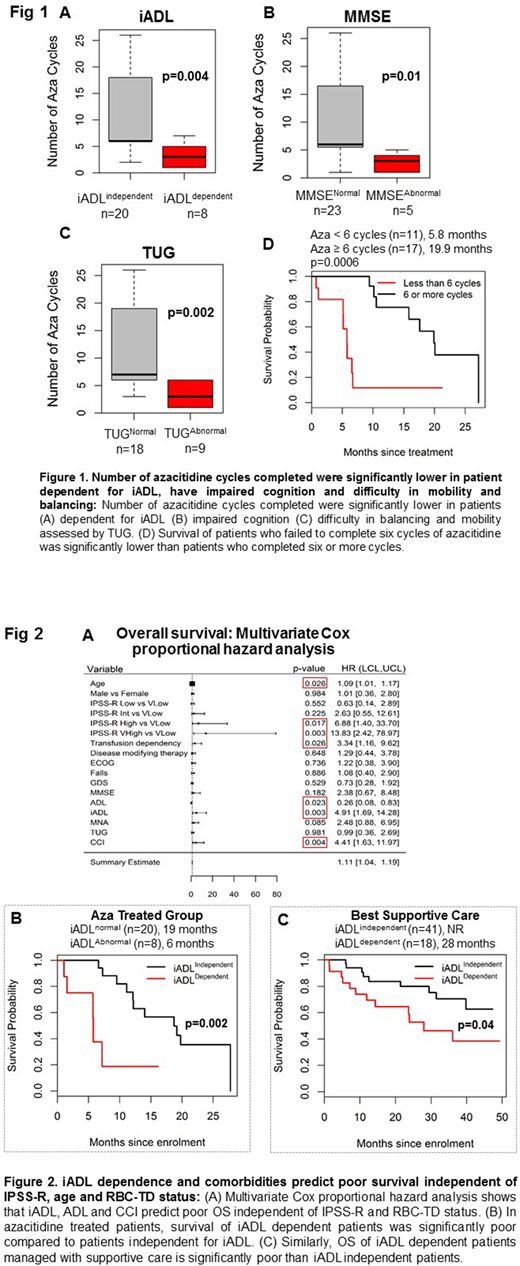
A total of 108 patients were enrolled into the study over a 4 year period. Although only 29 (27%) patients had an Eastern Cooperative Oncology Group score ≥2, 86 (79%) patients had deficits in at least one domain of ageing. Deficits were spread across all domains, including dependence for instrumental activity of daily living (iADL) (n=32, 29%). Patients who were iADL-dependent (3.2±5 vs. 10.8±15; p=0.004), were cognitively impaired (2.8±4 vs. 9.9±15; p=0.010) or had impaired mobility measured by the timed-up and got test (3.3±5 vs. 11.±15; p=0.002), completed significantly less cycles of azacitidine therapy than patients without deficits in these domains (Fig 1A-C). The patients who ceased therapy prematurely (less than 6 cycles) also had significantly poorer overall survival (OS) of patients compared to patients completing at least six cycles of azacitidine. (Fig 1D).
Other domains predictive of poorer survival were iADL dependence (HR 4.91; p=0.003) and increased comorbidities (HR 4.41; p=0.004) independent of age and disease factors (n=108) (Fig 2A). Additionally iADL dependence was associated with shortened survival regardless of therapy choice reflecting the frailty of this group of patients - azacitidine (6 vs. 19 months, p=0.002) and supportive care cohorts (28 months vs. not reached, p=0.04; Fig 2B-C).
Seventy patients were reviewed by the Geriatrician which led to the identification of a significant degree of multimorbidity (87%) and polypharmacy (73%), which have been shown to negatively impact on morbidity. Interventions and recommendations included changes in medications (57%), investigations for further evaluation of non-oncologic conditions (61%), social support referral including Aged Care Assessment (34%), nutritional support by counselling or referral to dietician (37%), formal cognitive evaluation and management (60%), physical therapy program referral or counselling (39%), referral or shared care with other specialists besides haematology and the primary care provider (26%), and psychologist referral (16%).
Conclusion:
This study demonstrates that geriatric assessment is feasible and instrumental in identifying geriatric related health issues in a significant proportion of patients compared to the use of performance scores. Deficits associated with ageing are associated with premature cessation of therapy and poorer survival. Geriatric assessments should form part of the assessment of older persons with the aim of reducing adverse outcomes and maintaining quality of life.
Ross:Celgene: Research Funding; Novartis: Consultancy, Honoraria, Research Funding, Speakers Bureau; BMS: Honoraria. Hiwase:Novartis: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal